By now you’ve likely heard something about the outbreak of food-borne illness due to E. coli that is currently causing problems in Germany. This outbreak, reportedly the world’s largest due to E. coli, has so far killed 15 people and left more than 1000 others ill.
Although the exact source of the virulent strain of this bacterium remains unknown, the pathogen has been identified on cucumbers imported from Spain. Specifically it has been identified as Shiga toxin-producing E. coli (STEC) which causes Hemolytic Uremic Syndrome (HUS).
Vegetables, however, don’t have colons for colonization with this bacterium, so how did they become “infected”?
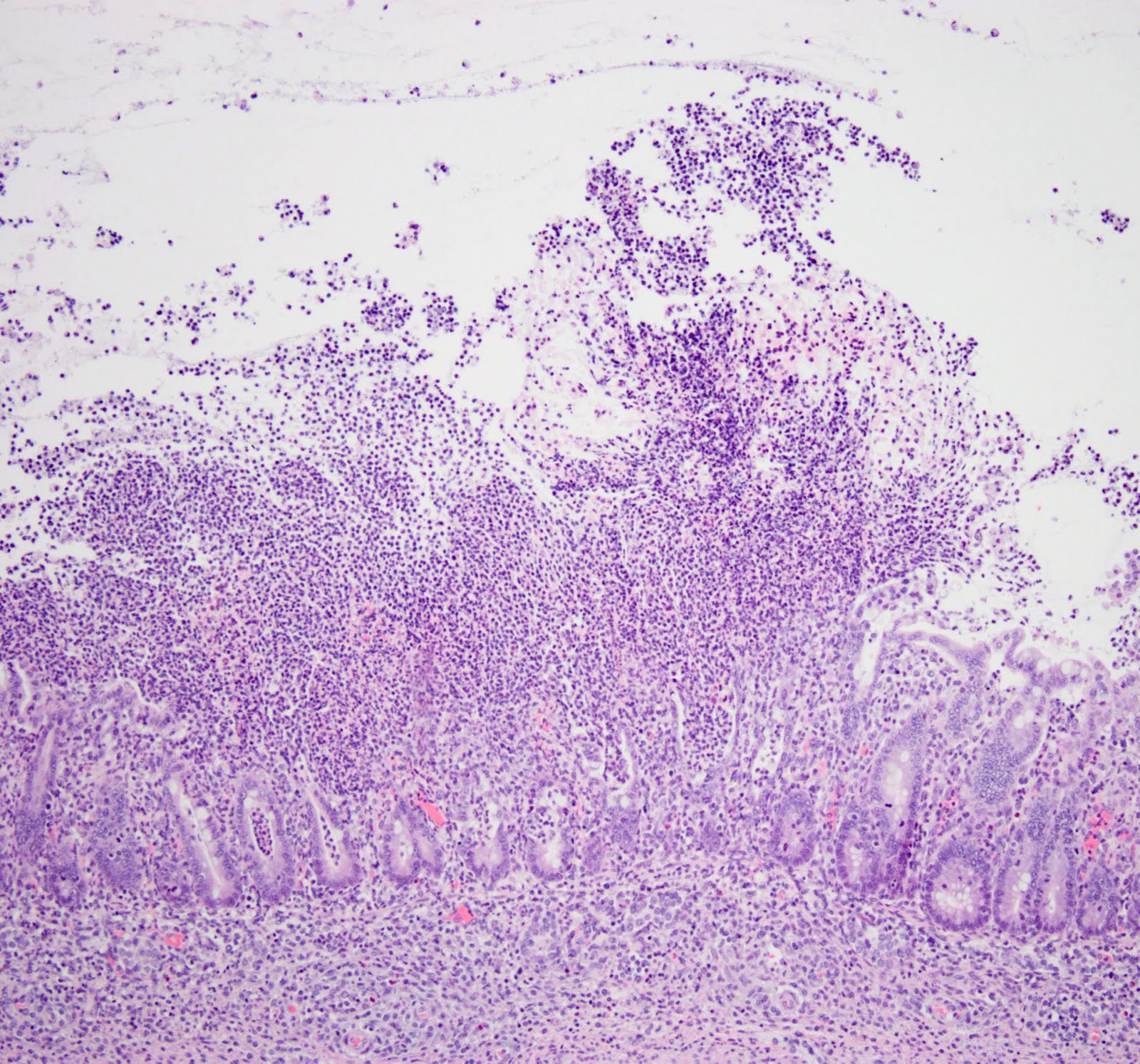
STEC and HUS
Most research on the epidemiology of STEC in animals has involved E. coli 0157:H7, and cattle are considered the major reservoir of the STEC that result in human infection. This strain is so widely distributed among cattle that it may likely be present periodically on most farms at some stage. Although this pathogen can only survive transiently in soil when shed by affected cattle, it is, however, capable of prolonged persistence in manure and environmental waters.
Consequently, polluted groundwaters may have been the source of the bacterium in this outbreak, and the vegetables were merely vectors of disease. That is, they provided a mechanical means of transporting the STEC into people.
HUS typically begins with an episode of bloody diarrhea following infection of the gastrointestinal tract with E.coli 0157:H7. This pathogen produces toxins that destroy red blood cells and cause kidney damage, resulting in a combination of hemolytic anemia, thrombocytopenia and acute renal failure. HUS therefore represents a medical emergency, and although the majority of patients recover from illness, mortality rate can be up to 10%, with children and the elderley being particularly at risk.
Growing Tension
Sadly this recent STEC/HUS outbreak has additionally spread to other northern European countries, and the situation is expected to further worsen in the coming week. Subsequently, diplomatic tension between Germany and countries such as Spain, France and Russia, is rising, as some countries have banned vegetable imports from Germany and Spain.
The German public has now been warned to avoid eating raw vegetables, such as lettuce, tomatoes and cucumbers, and some products have even been removed from store shelves.




Follow Me!